EMPHN ISIA Activity Update
EMPHN’s Quality Improvement (QI) model integrates clinical education, quarterly QI activities, resources, and clinical audits (under development) to enhance general practice. As part of their ISIA training, EMPHN initiated a Cancer Screening Campaign, focusing on cervical screening and promoting HPV self-collection. Data revealed that 43.0% of eligible people aged 25-74 had up-to-date cervical screening records, while only 36.8% of practices were connected to the National Cancer Screening Register (NCSR).
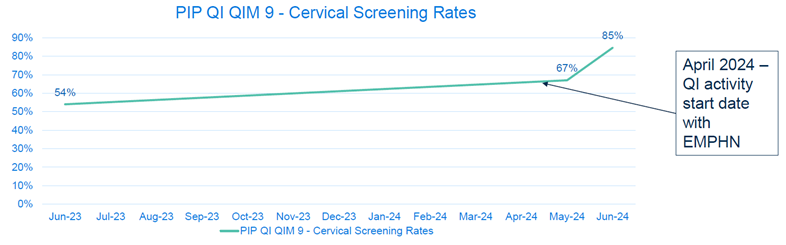
A solo GP clinic, opened during the 2020 lockdown, faced challenges with an inefficient reminder system due to merging of patient data, new patients and the challenges of the pandemic. The practice had an outstanding management, administrative and nursing team, however, during the last few years they had to function with a solo male doctor that had its inherent complications and barriers to cervical screening. The practice aimed to reduce the time needed to identify under-screened patients and promote self-collection to overcome barriers to accessing screening. The goal was to increase screening rates from 67% to 90% by September 2024. Key measures included the percentage of patients accurately recorded as screened within the past five years (PIP Quality Improvement Measure (QIM) 9).
Improvement strategies involved identifying improvement areas, preparing data to develop an accurate list identifying people who are overdue for screening, readying the team and practice, and enhancing participation in cervical screening for priority populations. Activities included practice nurses capability building by completing cervical screening (self-collection) training, integrating clinical software with the NCSR, conducting a QI research project, and updating cervical screening status in patient records.
As a PHN team when we went to the practice to implement the QI we observed the following challenges:
The practice team had started their improvement journey in 2023 and had already implemented many activities that had led them to an increased screening rate. They knew that they were doing a good job, however, their practice data (PIP Quality Improvement Measure 9) was not reflecting the improvement efforts.
How we overcame those challenges:
The EMPHN team supported the practice to complete a process mapping activity that highlighted their process improvement activities and practice workflows (refer to diagram 1). This provided the practice team with an opportunity to identify barriers and together brainstorm further ways to solve issues and identify new areas for improvement.
The team showed interest and were excited in the following approaches:
From the mapping activity, the practice was able to identify new ideas to be tested, including activities leading to improved recording of completed cervical screening in patient files that had a significant impact on their PIP QIM 9 data (ref to diagram 2). As a result of this valuable mapping activity, the practice is now implementing activities that will support sustainability of the hard work completed to ensure an ongoing focus on improved patient health outcomes. The practice is now taking their learnings into their next QI activity focusing on Bowel Cancer Screening.
As a PHN we had the following learnings from the ISIA project that we would like to incorporate in other QI initiatives we undertake with the general practices:
Undertaking quality improvement activities requires time and many practices face barriers impacting opportunity to allocate the required protected time needed to initiate activities. The ISIA project highlighted the role that PHNs play in assisting practices with the initial planning stage to develop problem and aim statements and initiate discussions to identify barriers and key drivers to support successful improvement activities.
Achievements included co-designing with the practice team, contributing to EMPHN QI refresh, and planning sustainability actions. The project underscored the importance of effective data management, team training, and leveraging technology for efficient patient identification and engagement.
Diagram 1: Improvement Idea 1: Process mapping to Identify areas for improvement.
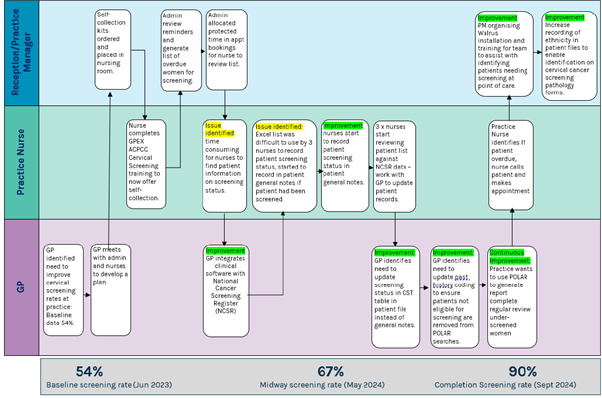
Diagram 2: Practice Improvement